Increasing air pollution combined with the rising number of patients with immune system deficiencies has become a serious problem within the Hospital Environment.
There is a huge price to pay for airborne infections, both in terms of human life and financial costs.
Consequently there is a general need to ensure that the air in the hospital environment – in all parts of the facility – is of the highest possible quality.
To come to the right decision with regard to air purification one of the most important requirements to be met is thoroughness : all pollution must be eliminated from the air.
There is no point in cleaning the air just a little bit.
In illustration of this, a survey of ‘air’ is annexed which outlines the size of pollution, the way in which it is measured, and the method to eliminate pollution.
From the survey of causes and sorts of pollution, there are only two kinds of pollution:
1. Solid elements (Particles)
E.g. dust, pollen, diesel smut, bacteria, viruses etc.
These particle pollutants can only be removed effectively and efficiently through a High Efficiency Particulate Air filter or HEPA filter, or a higher quality filter such as ULPA
It is important to take into account that 99.9% of all airborne particles are smaller than 1 µm (micrometer). 1 µm = 10-3 mm = 0.001 mm.
So if the filter specifies removal of airborne particles up to 1 µm, the air is only being purified of 0.1 % of the total pollution. A high degree of efficiency is required of the filter in order to perform adequate air purification.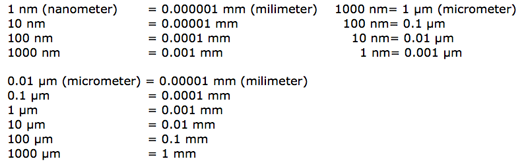
2. Gases, smells and chemical compounds
E.g. organic like acetone
E.g. inorganic like ozone
These pollutants can only be removed by filtration through activated carbon.
Thus the filter cartridge of air purifiers must contain both of the above mentioned filters in order to perform efficiently. Other important technical aspects are:
The volume of air (in M³/H) which can be processed in a certain period of time. (capability – capacity). In practice the influx of pollution is hardly ever steady, but rather variable. Therefore the time span necessary to perform the purifying process is important, especially when there is heavy pollution (e.g. labs).
The way the polluted air is sucked in the device and the position of the device in the room. (breathing zone)
The way in which purified air is being released, how the blending of clean and polluted air takes place. (airflow pattern)
In short:
What is airborne pollution?
Airborne pollution is only 2 things: Particles and Gases.
What are Particles?
Particles are like dust. They are big (like sand dust or e.g. smoke coming from burning oilfields which can be seen by the human eye) to smaller and smaller – up to the size of bacteria and viruses (which of course, cannot be seen by the human eye)
How can we take these particles out of the air?
Particles are being removed from the air by means of a filter system. It depends on the efficiency of the filter system and its other capabilities of how much or how many or how small particles are being removed out of the air.
What are Gases?
Gases consist of chemical compounds; each gas has its particular chemical combination.
How can we take these gases out of the air?
Gases are being removed from the air by means of a filter system based on activated carbon.
How can we remove these 2 things – particles and gases – out of the air?
You need a filter on HEPA basis and an activated carbon filter. The HEPA filter (level 14) is necessary because that is the most efficient type of HEPA-filter (takes out everything up to bacteria and viruses) and has an individual leak-test on every filter cartridge. A lower type of filter will not be as efficient, will consequently not take all pollution out of the air and will not contribute to the human health as needed within the medical world.
Note: All professional air filtration systems in e.g. clean rooms, laminar flow, closed HEPA circuits, use the mechanical technique (= HEPA filters), like MedicCleanAir® does.
The reason for this:
- a continuous optimum efficiency (high efficiency during a long period of time)
- no side effects (like creation of ozone, etc)
To learn about other filter techniques and why these are not efficient, go to other FAQ.
A decrease or removal of problems caused by indoor air pollution can only be realized if the apparatus meets with certain imperative technical facilities.
The most important condition is that all pollutants (particle as well as gaseous) must be eliminated from the air with a high efficiency for prolonged periods of time.
There are also other requirements to be met which are discussed hereafter.
All requirements must be completely adjusted to each other.
1. Filter specifications
a) Effective Pre-filter to protect the Activated Carbon -filter
The pre-filter must be a fine dust-filter with the highest normative results in this class of filters. If these norms are not met the pores of the activated charcoal filter will quickly become choked up whereby the efficiency of adsorption will decrease fast and will even disappear.
b) Activated Carbon filter with high adsorption power
The activated carbon-filter must have a large adsorption surface in order to work efficiently during a prolonged period of time.
c) High-Efficiency Particulate Air filter or HEPA filter
It is important to take account of the fact that 99.9 % of all airborne particles are smaller than 1 µm (micrometer). 1 µm = 10-3 mm = 0.001 mm.
So, if the filtration norms are up to e.g. 1 µm, then only 0.1 % of the total pollution is being purified.
The capacity must be extended to much smaller particles in order to eliminate cigarette smoke, bacteria and viruses (0.1 – 0.01 µm)
2. Efficiency
Given absolute purification of the air it is important how many M³ of clean air can be produced per hour, not only to maintain a satisfactory level of purification but also to – if necessary – clean the air of a room in a short time span when additional pollution has occurred.
3. Optimal action for air intake and release
Optimal air cleaning is only possible when the polluted air is being extracted from all sides (= over 360°) and when the purified air is maximally blended with the remaining air in the room (= the supply of clean air over 360°)
4. Mobile in order to be used whenever and wherever necessary
Pollution is not always concentrated at the same place. In practice it may be necessary to move the device to another location to perform extra air cleaning in that location.
5. Low energy expenditure
Effective air purification is only possible when it takes place permanently, 24/24 hours, 365 days/year.
Taking the energy cost (electricity) into account, this requirement is clear.
6. User friendly
The user must not be obliged to regularly clean or change filters, add certain products or items, etc.
A device that requires frequent maintenance will easily be turned off or taken out of operation.
7. The air cleaner itself may not be a source of pollution
Both the device itself as its method of air purification may not be a potential source of pollution, during or after use.
a) During use
Applying non-mechanical techniques can cause additional pollution. A well-known example is the creation of ozone by electrostatics or ionization and the formation of micro-organisms by humidifiers.
If products contain a large amount of synthetics (plastics), in the course of time emission of PCB (polychloric biphenyls) may take place. Patients are not to be surrounded by polluting effects or materials.
b) After use
The environmental demands with regard to recycling and waste practice are becoming very strict. The device, accessories and filters should be as environmental friendly as possible.
8. Operational in a low noise environment
It is clear that the Mobile HEPA Unit must be able to perform efficiently with low noise dB in the surroundings of patients and staff.
9. Alarm
That controls the performance of the filter cartridge, controls the hygiene security, pressure difference and informs about the level of saturation of the filter cartridge at any time.
The sole reason why MedicCleanAir® was started in Switzerland in 1998 is that the following questions could not be answered:
"How come that Hospital Infections are such a problem all over the world, that there exist very cheap mobile purifiers on the market, and that there are obviously no devices installed in the critical areas of the hospitals to avoid these infection problems?" (although large multi-nationals have such 'air purifiers' on the market and sometimes at very low prices)
"How come that when I have a child that suffers daily from allergies or asthma (problems due to airborne pollutants), and when I go to the doctor for advice, that this doctor does not say that I have to install purifier X or a Y in his/her bedroom?"
The answer:
The low budget air purifiers (based on water purification, ionisation, electrostatics, ultra-violet), sometimes manufactured by big companies, have no extensive and published medical support. The reason is that these air purifiers are not efficient enough to eliminate bacteria, viruses, fungi, etc. on a constant and long time basis.
Consequently 'patients' do not benefit from the implementation of these air purifiers. In other words: those air purifiers are a waste of money.
It is different with MedicCleanAir® – Mobile HEPA Units.
MedicCleanAir® – Mobile HEPA Units have obtained the medical support through multiple medical, clinical and laboratory studies carried out during a long period of time in real hospital circumstances.
When evaluating the market of air purifiers or mobile HEPA units, it is very important to ask the manufacturers for the medical tests that have been carried out and published by (serious) hospitals/universities. These medical/clinical tests must be published on a world-wide basis by leading medical organisations such as the Hospital Infection Society or Bone Marrow Transplant.
In fact, the only reason why MedicCleanAir® started to investigate the market of Mobile HEPA Units was that undersigned lost a family member due to a hospital infection. In other words: the operation went perfectly well, but the patient got infected afterwards and unnecessarily lost his life.
Starting with the help of the University of St. Gallen in Switzerland and going through a lot of medical tests and advice during the last decade, MedicCleanAir® has come up with a Mobile HEPA Unit that can count on the support of the Medical World.
It resulted in a range of products of which the MedicCleanAir® PRO and ISO series are unique for the Medical World.
Hendrik Van Passel
Managing Director
Apart from the medical considerations, also the financial aspects play an important role.
What can a hospital / department save when MedicCleanAir® is installed?
Firm statements on price comparisons are very difficult to submit as healthcare systems differ per country.
The listed financial considerations are aimed to enable general financial comparisons in specific (local) circumstances.
Example 1: Dept. Haematology/Oncology
These patients are at (high) risk for infections and are given preventive medication to decrease the risk of an infection, mainly Invasive Aspergillosis.
For an average department in Europe (20 patients) the cost for this preventive medication amounts to around € 500/day/department (not included the medication for highest risk patients of up to € 200 – 300/day/patient – antimicotica).
Fixed annual budget required for this preventive medication is around € 180.000 to € 200.000 every year to fight airborne infections, mainly Invasive Aspergillosis.
Despite this preventive medication the risk of an Invasive Aspergillosis Infection still remains.
Treatment costs of an Invasive Aspergillosis infection is over € 30.000.
When the MedicCleanAir® instructions are followed, airborne CFU's will be eliminated.
The required budget to achieve this goal in a department with 20 patients is less than € 40.000. This budget is calculated on a 3 year-basis with a confirmed technical guarantee and price guarantee.
In other words: Annual savings of minimum € 160.000.
(See also test results regarding clinical, medical and laboratory test Bone Marrow Transplan 2002 – Clinical study Cuneo-cost benefit analysis)
Example 2: Operating Department / Operating Theatre
With the MedicCleanAir® concept, at least one question becomes less important.
Where do infections occur?
Is it in preparation, on the operating table, in the O.T. or in recovery?
With MedicCleanAir® there should be no real financial discussion anymore about where to submit clean air in the operating department.
Operating Theatre
In O.T’s, clean air (without CFU's) is required at all times, and MedicCleanAir® is a serious economic option to achieve this goal.
The 3 valid reasons to consider MedicCleanAir® for O.T.'s are:
- The total elimination of airborne CFU's in the complete area of O.T. (including the 'jumper areas’)
- The required initial budget (no MedicCleanAir®) is a lot higher than the one MedicCleanAir® offers,
- The required operational budget with MedicCleanAir® is far less than the operational budget of the alternative.
With MedicCleanAir®:
For an average O.T. the required budget is around € 16.000.
For an average O.T. the required operational budget is less than € 40/day.
This budget is calculated on a 3 year-basis with a confirmed technical guarantee and price guarantee.
Operating Department:
To get Clean Air in the total operating department (including 2 O.T.'s and jumper area’s) the required initial budget amounts to less than € 40.000.
For detailed information on your specific situation, contact MedicCleanAir®.
What are the benefits for the patient when MedicCleanAir® Mobile HEPA Units are implemented in the hospital facilities:
- Reduced risk of infections (with all possible negative consequences up to death)
- Can go to work faster because stays less time in the hospital
- Less family pressure because can go home more quickly
- Less financial pressure because he/she still has to pay (partly) the medical costs
What is the benefit for the hospital when MedicCleanAir® Mobile HEPA Units are implemented:
- The hospital complies better to the government directives in relation to good medical care
- The hospital reduces waiting lists for patients, so more turnover for doctors/specialist and the hospital
- Approx. 25% of all patients in ICU’s are infected and a pneumonia infection means between 6.8 and 30 days of prolonged hospital stay – average costs per patient about € 10000.–
- Better facilities and image – Patient Care – competition between hospitals
- Can produce better figures to Governmental institutions – less lay days
- Less work pressure on (sparse) hospital staff
- Less psychological pressure on hospital staff (working with patients that die in the end)
- Less chance for hospitals to close down entire departments due to an out brake (which happens far more than we all think it does, with a price ticket of € 500000.– to € 1000000.– per case of closing down a department)
- No closing down of departments due to renovation works when MedicCleanAir® Mobile HEPA Units are chosen instead of renovating integrated HVAC circuits with HEPA filtration = far smaller investment.
What is the benefit for the Government when MedicCleanAir® Mobile HEPA Units are implemented:
- Reduction of the general overall patient cost, because patients go home more quickly
- Reduction of the general drug costs (less anti-biotica before/after infections)
- Patients go to work more quickly which means that through labour, the government gets more income, more taxes, and spends less money on social security, etc. (macro-economical)
Conclusion:
Clean Air in Hospitals is not a luxury – it is a must!
For detailed information on your specific situation, contact MedicCleanAir®.
The importance of the airflow in a room in relation to the reduction of hospital infections is illustrated in the drawings below.
The drawing is based on an average patient room in an average hospital in Europe. The example is given to explain the importance of airflow.
We take a normal patient room with air supply through a grid above the entrance door and air extraction is done through a grid in the bathroom.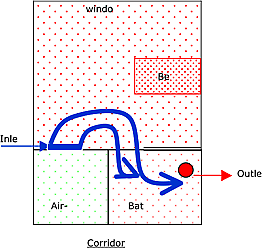
As can be seen on the drawing:
The air being blown at the entrance into the room by the ventilation system is nearly entirely sucked away by the extraction grid in the bathroom (blue arrows).
This example is given to explain that it is not only important to have input and output of air, but that the ability of the air of reaching all corners of the patient’s room is of prior importance as well.
In other words: the airflow pattern is of prior importance because if not, the patient will not benefit at all from the supplied clean air.
Airflow patterns for Mobile HEPA Units:
It is clear that a Mobile HEPA Unit should be capable of creating an air stream in such a way that its purified air is going to all corners of the patient’s room, and that all polluted air is extracted from all corners of the patient’s room.
Additionally, the position of the Mobile HEPA Unit in the room and its technical characteristics must be of such that the priority of supplying clean air to immune-compromised patients is met, where in the case of infectious patients the priority lies with extracting polluted air arising from those patients.
In other words:
The power of the air current should be strong enough to reach all corners, but at the same time at a comfortable airspeed for the patient (see drawing), something that is considered to be very important in Europe - do not create a storm over the patient(!)
The proof that a Mobile HEPA Unit has the correct airflow pattern can only be given by
- scientific proof (engineering) and
- medical proof (international medical organisations)
The MedicCleanAir® Mobile HEPA Unit and Airflow Pattern:
The MedicCleanAir® airflow pattern and its effectiveness has been scientifically proven by
- the University of Leuven, Belgium: the MedicCleanAir® Mobile HEPA Unit creates an airflow that extracts existing/polluted air and supplies all corners and parts of the patient's room with HEPA filtered air within 8 to 12 minutes.
- numerous publications from Scientific Institutes and University Hospitals in various countries (more than 8 different organisations up to now !)
The MedicCleanAir® Mobile HEPA Unit eliminates airborne contamination under normal hospital working conditions, as well as under extreme conditions (renovation works, etc.).
One can clearly see that contaminated air is extracted from the patient’s breathing level (drawing on right hand side) and that HEPA purified air is supplied to the patient’s breathing level (left drawing). The velocity (airspeed) of the air can be seen only on the colours of the left hand side drawing (0.1 à 0.4 m/s is considered to be comfortable). Colours of right drawing are not in relation to the airspeed bar.
The airflow pattern of the MCA unit in a patient room - University Leuven (B).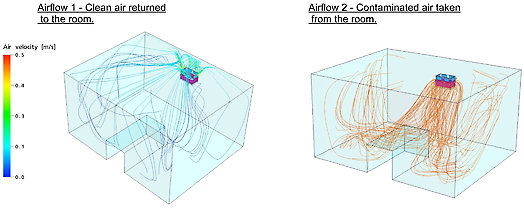
edicCleanAir® Mobile HEPA Units and the importance of the breathing zone in relation to infectious patients and immune-compromised patients
1. Infectious patients (TBC, SARS, H5N1, pox,…) and MedicCleanAir® Mobile HEPA Units
The place to install the MedicCleanAir® Mobile HEPA Unit for infectious patients = next to the patients bed.
The air that the patient is breathing out is captured as quickly as possible as it contains infectious agents. Additionally, hospital staff and visitors that are entering the patient’s room, breathe clean air.
See red lines (= air being sucked into the Mobile HEPA Unit).
Source: University Leuven – Belgium – Biosyst MeBios Department.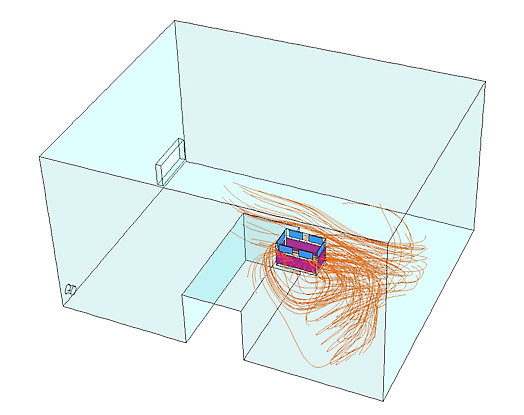
Direction and velocity of the air at the level of the head of the patient (bed):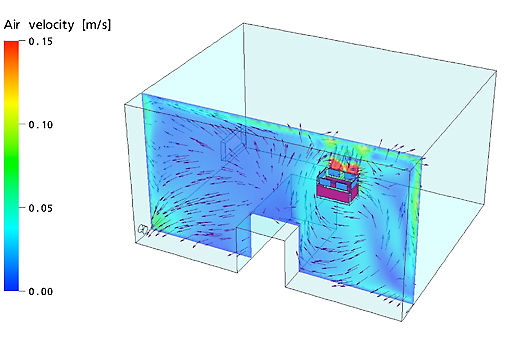
2. Immune-compromised patients and MedicCleanAir® Mobile HEPA Units
The air that the patient is breathing in needs to be as ‘clean’ as possible. It is therefore a plus-point that the air coming out of the Mobile HEPA Unit (= clean air) is going to the patient as directly as possible. Place to install the MedicCleanAir® – Mobile HEPA Unit for immune-compromised patients = opposite the patient’s bed.
MedicCleanAir® Mobile HEPA Units make use of the ceiling of the room to supply the patient with HEPA filtered air. See blue lines (= clean air coming out of the MedicCleanAir® Mobile HEPA Unit, going to the patient by using the ceiling)
Source: University Leuven – Belgium – Biosyst MeBios Department.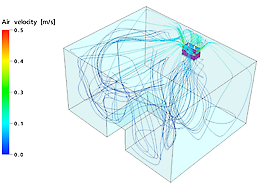
Direction and velocity of the air at the level of the head of the patient (bed):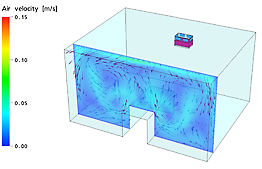
Good to know:
The air consumed by an average patient (normal resting condition) is less than 3 M³ per hour.
The amount of air that MedicCleanAir® Mobile HEPA Units purify in rooms with infectious patients, or the amount of HEPA filtered air that MedicCleanAir® Mobile HEPA Units provide to immune-compromised patients is x 80-times to what they pollute (infectious patients) or to what they consume (immune-compromised patients)
CDC prescribes air changes hour (ACH) for fixed installations. When one applies these rules for Mobile HEPA Filters, MedicCleanAir® can provide you with the required ACH with their New Generation Mobile HEPA Units.
Other airflows: (NOT MedicCleanAir®)
Floor standing units create vertical airflow patterns with air-intake at the top and air-outlet at the floor level (or visa versa).
An air purification unit with a vertical airflow does not lead to a significant decrease of airborne infections because these air purification units are not capable of creating an airflow in a patient's room, as several medical studies have clearly proven.
In several cases, these floor standing purification models needed additional fans in the test rooms to disperse the air coming from these units in to the test room.
In some cases, E.g. intake at top and outlet at floor level, the dust and cfu on the floor are made airborne again.
All floor standing models take valuable space and are in the way of everybody.
The vertical airflow of a certain mobile HEPA unit in a room with a bed: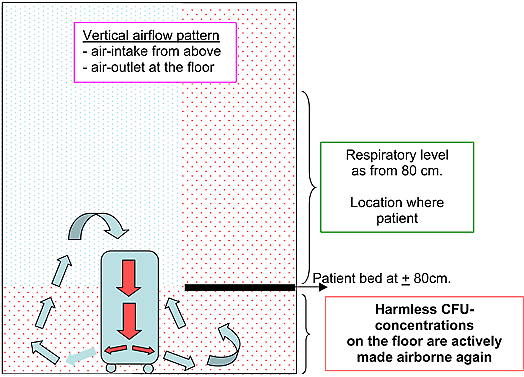
Conclusion:
It is not only necessary to manufacture a mobile HEPA unit that has “efficient filter cartridges”. The airflow pattern it creates must be correct or the “infection control unit” becomes even dangerous to the patients in medical centres – as shown above with vertical airflow patterns.
in the MedicCleanAir® Mobile Hepa Units
Why do you have 3 filter systems in your filter cartridge?
Pollution in the air consists of only 2 things: particles and gases. There is nothing else. So, by eliminating 2 as much as possible, one has an efficient air cleaning device. For the particles, MedicCleanAir® has the most effective HEPA level (level 14) and ULPA 15 level, and for the gases the activated carbon. The pre-filter F9 is only integrated as a protection for the activated carbon filter.
Why not integrate these 3 filter types separately ? Why putting or joining them all together in one filter cartridge?
By putting them together in a special way, MedicCleanAir® obtained the highest efficiency possible. Additionally, by separating the 3 different mediums, maintenance would be costly. One could be required to change pre-filter after 7 months, the activated carbon filter after 10 months, the HEPA or ULPA filter after 1.3 years. This would create an enormous maintenance cost.
How long will the MedicCleanAir® filter cartridge last?
An alarm (LED) informs the client to change the filter cartridge in case of saturation. The time lap to reach saturation depends on the type and quantity of contamination. Extreme circumstances, for example renovation works (lots of dust) will shorten the life time of the filter cartridge. In those circumstances, MedicCleanAir® recommends the use of additional pre-filters to be installed on the outside of the Mobile HEPA Unit. These additional pre-filters are disposables and can be changed regularly.
When used in normal hospital circumstances, the MedicCleanAir® filter cartridge is efficient during 12 months.
What will happen when the filter is blocked by pollution, or when it is saturated by particles?
The air that comes out of the MedicCleanAir® Mobile HEPA Unit is clean HEPA filtered air at all times. When the filter cartridge becomes more and more blocked or saturated by particles, the pores of the filter cartridge will be filled and blocked. This results in the fact that when the filter cartridge becomes saturated, less clean HEPA filtered air (less quantity) will come out of the MedicCleanAir® Mobile HEPA Unit. So, less air but same quality (or even better).
As from 2007, the MedicCleanAir® Mobile HEPA Units are equipped with an alarm that informs the client to replace the filter cartridge.
Note: should the alarm go of before 12 months have passed in ‘normal hospital working circumstances’, the hospital really has a problem with airborne contamination in its critical area’s.
What happens to bacteria, viruses fungi in the filter cartridge? Are these captured by the filter cartridge? How long do they stay alive? Can they pass through the filter cartridge?
Bacteria
Bacteria in general need to have a basis of nutrition together with an ideal breeding ground in order to survive. In other words: bacteria on themselves cannot survive on an active basis without its nutrient basics, the ideal temperature and humidity needed for that specific bacterium. Nutrient basics can be water, “white of eggs”, etc. As long as the bacteria can feed itself with its nutrient, it can continue to exist, grow and/or multiply itself, be active.
The basic, or possibly the nutrition itself can be airborne through e.g. particle, droplets, or even human tissue. (E.g. TBC, pox, measles) When, trough air purification, the basic and the bacteria specie are being captured, held and kept in the filter cartridge, the bacteria specie will stay ‘alive’ until all nutrients are being consumed (and no other nutrients are being proposed to that specific bacterium). Also the perfect ‘breeding ground’ (= temperature, humidity …) is needed to keep bacteria active. When this perfect breeding ground fails to exists, when the bacteria species run out of nutrition, when temperature or humidity are not ideal, they die. A small number of them however may continue to ‘live’ in ‘sleeping circumstances’, they are in a non-active condition. However, major requirement for this ‘sleeping condition’ is that the ideal breeding ground (temp./humidity, etc) is kept. If that is not the case, they will die as well.
Viruses
Viruses are intracellular species; meaning that they cannot exist out of the environment of a cellule or cluster of cellules. The virus needs the cellule(s) for its nutrition, its survival, together with – as said for bacteria – the perfect breeding ground – temperature, humidity etc. They can only survive when multiple cellules are being presented to the virus itself. A virus cannot multiply itself without the availability of cellules. As soon as the virus runs out of its nutrient, it dies.
Cellules and their accompanied viruses, when transported through the air, are being absorbed by the MedicCleanAir® filter cartridges. The viruses will stay ‘alive’ until all nutrition from the cellules or cellule clusters has been ‘consumed’. Consequently, they will die after that.
Time lap during which bacteria and viruses will remain active
The exact time lap in which bacteria species and viruses can remain alive or in ‘sleeping condition’ is difficult to determine. It depends on which and how much nutrition that specific bacteria specie or virus has at its disposal at that specific time. Consequently, one can state that the same species, airborne with a cluster of e.g. water droplets will remain longer ‘alive’ as another specie of the same type, airborne with a smaller number of e.g. water droplets.
It is therefore impossible to determine how long a specific specie will remain alive within the filter cartridge.
All specialists however are determined that the time of survival for either bacteria species or viruses without any nutrients is between several hours and few days. Survival during several months or years is practically 100% excluded. Nevertheless bacteria spores in ‘sleeping conditions’ are the oldest life form on earth and no exact data is available on how long these might be able to stay in their ‘sleeping condition’.
However, the efficiency of the MedicCleanAir® filter cartridges secures the capturing of bacteria and viruses at all times.
Fungi/Aspergillus
Fungi are specie which is a life form on itself. It grows without the need of a basic nutrient. It grows – multiplies when living in the correct temperature and humidity. Some are more active than others whenever in ideal situations. They are sized between 2 and 10 microns and are transported through the air without any means of a ‘transport/carriers’. Aspergillus is found everywhere; in normal houses, outside in open air, in office buildings, in hospitals, on floors, walls, ceilings, in HVAC-systems, heaters, furniture, in dust, etc. Healthy people exposed to these fungi, do not experience any difficulty or health problems. However, immune compromised patients (which have an immune deficiency) can die from being exposed to fungi (I.A. Patients). It is therefore that optimum air cleaning in patient rooms is of utmost importance.
Further info and different kinds of fungi can be found on:
http://www.aspergillus.man.ac.uk
Capturing of bacteria and viruses through air purification by MedicCleanAir®
Bacteria species and viruses need mostly ‘carriers’ to transport themselves to other nutrition grounds. These carriers (dust, tissue, droplets …) have a certain dimension. The efficiency of the filter cartridge determines whether a certain ‘carrier’, be it particle, or droplet, or something else, will be adsorbed or not.
The MedicCleanAir Mobile HEPA Unit has 100% efficiency on particles of 0.3µm and larger.
Additionally, the MedicCleanAir® Mobile HEPA Unit has been tested on particles which are 30x-times smaller than 0.3 microns. The efficiency of the Mobile HEPA Unit on particles of 0.017 microns is 99.27%. – See test results scientific –
In other words: the risk that something can pass the MedicCleanAir® Mobile HEPA Unit is 0% on 0.3 microns and limited to 0.7% on 0.017 microns. Furthermore if any should not be adsorbed, the chance of recapturing the contaminant is 99.3%!
Conclusion
The efficiency, capturing or break-through of pollutants is not to be discussed for particles of size of 0.3 microns and bigger. The results are 100% positive, 100% adsorption.
As far as the carriers of bacteria and viruses smaller than 0.3 microns are concerned the MedicCleanAir® Mobile HEPA Units have an efficiency of over 99% adsorption capability as shown multiple medical tests – see test results medical –
How to dispose of the filter cartridges?
The filter cartridges used in normal hospital working conditions go with the normal waste procedures of the hospital to waste factories (to be burned).
However, in some circumstances the filter cartridges have to be treated differently. Example for this is when the MedicCleanAir® Mobile HEPA Unit has been used during the preparation of cytostatic products in pharmacy labs. Cytostatic products are being used to make drugs for patients with cancer. Cytostatic products are toxic themselves, and become airborne (gas) at normal room temperature. MedicCleanAir® Mobile HEPA Units are installed in such preparation rooms because the normal safety cabinets are not equipped with activated carbon filters (necessary to adsorb gases). When MedicCleanAir® Mobile HEPA Units are implemented in these labs, the filter cartridges adsorb these toxic gases, and have to be disposed of through the channel of toxic waste of the hospital (which exists in every hospital)
Conclusion: usually, filter cartridges are disposed through normal waste procedures
Where do we have to change the filters cartridges?
In the basement of the hospital or outside the hospital. The maintenance or changes of filter cartridges are never to be done within the area of use. But, these instructions are also mentioned in the manual which accompanies each unit.
Does MedicCleanAir® have other types of filters?
Yes, see products
Is there any other maintenance for the machine then changing the filter cartridge?
No, normally not. Filter change after 12 months during which the inside of the machine (where the filter cartridge is placed) and the outside of the machine is disinfected. But, maintenance instructions are joined in the manual which is delivered with each MedicCleanAir® Mobile HEPA Unit.
Can the motor be contaminated?
No, the motor cannot be contaminated because the motor is installed in the area where HEPA filtered air is leaving the Mobile HEPA Unit. As such, polluted air is never in contact with the motor.
Why choose for stainless steel?
Stainless steel is mainly used in critical areas of hospitals because of its sterile capability. It is very smooth so that no contaminants can stick to it, and the MedicCleanAir® Mobile HEPA Unit is kept shiny because that way one can see everything on it and be sure that the surface is clean. However the latest MedicCleanAir® units are in epoxy white anti-bacterial coating – see also FAQ “mobile HEPA units can be contaminating themselves”
Do we need any spare parts for this machine?
No. Up to now, MedicCleanAir® has had no defects in any of the parts of the device.
Do we need to adjust the room or the department to install these devices?
No, the devices are stand-alone units. They suck the polluted air in, purify the air, and blow it back into the room of the patient or department. The unit is to be put on a shelf at 2/3rd of the height of the wall. Electricity to be supplied (220V), the unit to be turned on and not to be touched again during 12 months after which the distributor will change the filter cartridge and perform the maintenance. All MedicCleanAir® Mobile HEPA Units are equipped with an alarm that informs the client when the filter cartridge has to be changed.
Where in the room or department should we place this device?
It is to be put against the wall or on top of a closet (2/3rd of the height of the wall).
In case of infectious patients, close to the patient, in case of immune-compromised patients, opposite the patient’s bed, in case the origin of contamination is for example contamination coming out of the grid of a ventilation system, one puts the MedicCleanAir® Mobile HEPA Unit close to that grid. If the source of contamination comes through the door, put the machine next to the door or above it. – See also FAQ “Air flow patterns and the importance of the breathing zone” –
Does the MedicCleanAir® Mobile HEPA Unit have any influence on the heating, cooling, moistening or drying of the existing air present in the room?
No, the MedicCleanAir® Mobile HEPA Units purify the air. The device doesn’t do anything about heating or cooling, nor about moistening or drying the air. It is an Infection Control Unit – air purification device.
How long do we let the device running? Do we put it on or off?
24/24 hours, day in – day out: for 12 months, or as long as the alarm for filter change does not inform you that the filter cartridge has to be replaced. The reason for this is that contamination in hospitals comes from inside the hospital and to maintain a good air quality, the MedicCleanAir® Mobile HEPA Unit must always be operational. – See graphic red and blue in brochure – the machines were put on (contamination drops), contamination fluctuates (because doors opened to treat patients, etc.) and then the units were turned off. Result: contamination rises immediately. So, the MedicCleanAir® Mobile HEPA Units must be kept running at all time.
Summary V.I.T.O. – report: 2000/MIM/R/7 – MedicCleanAir® – nr. 991351.
MedicCleanAir® Efficiency on regular Indoor Air / all particle sizes / working conditions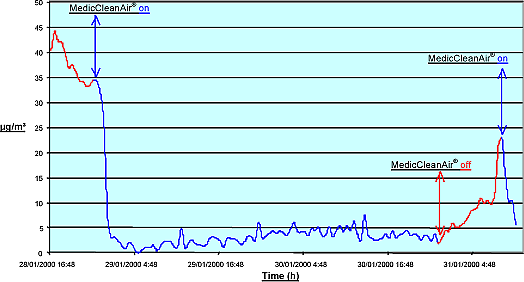
We have already fixed HEPA-ventilation systems in our hospital for certain ICU’s. Do we need MedicCleanAir® Mobile HEPA Units as well? Or can these help in case our existing HVAC-systems are not up to standards?
It is clear that integrated HVAC-systems which are equipped with HEPA filters are good systems and very often reach the necessary standards regarding air quality in certain risk departments. As all ventilation systems have to take fresh air from outside the hospital, it is the quality of the filters installed in these systems that will originally determine the air quality in the hospital or that specific department.
However there are some critical factors and limitations to the application of the HVAC-systems equipped with HEPA filters:
Maintenance:
Whenever maintenance including periodic filter change has not been carried out at a certain moment (usually at least once a year), all tubes of the HVAC-system are polluted with micro-organisms which are now free to develop, grow and/or multiply. Once the maintenance has been “forgotten”, the evil is done. This situation can be repaired/helped by the use of MedicCleanAir® Mobile HEPA Units.
Contamination develops inside the hospital:
Pollution or CFU’s develop inside buildings and rise as soon as activity is taking place in the area. As soon as people (patients, visitors or staff) are present in a certain area, contamination rises. The HVAC-systems equipped with HEPA filters try to reduce this contamination by suppressing the indoor air with HEPA filtered air. This takes a very long time and is often completely ineffective as there is no effective airflow.
MedicCleanAir® Mobile HEPA Units purify the air from inside and accomplish the task of providing the risk area with HEPA filtered air fast and efficient, as proven by multiple medical studies by several university hospitals. – See test results –
Immune compromised patients:
Immune compromised patients need to breathe HEPA filtered air. Therefore, the grids supplying the HEPA filtered air should be positioned in such a way that the HEPA filtered air coming from the HVAC-system is going directly to the immune compromised patient (breathing zone). This is in 90% of all patient rooms not the case. Additionally, very immune compromised patients are to be placed in rooms with positive pressure. Also this is in 90% of all cases not possible with the existing HVAC-systems of the hospital. The use and implementation of MedicCleanAir® Mobile HEPA Units solve this (these) problem(s). – See products, MedicCleanAir® – ISO Concept
Infectious patients:
Infectious patients breathe out or give off certain infectious species (E.g. Tuberculosis, (avian) influenza, SARS …). Therefore, the air in that risk area should be purified as quickly as possible. As HVAC-systems with HEPA filters use the technique of suppression, the air is not purified but suppressed from the risk area. Additionally, HVAC-systems often re-use a large percentage of the air in order to save money on heating and/or cooling. Very often, these HVAC systems do not have any HEPA filters on the extraction grids of the ventilation system so that infectious species are spread to the rest of the hospital.
Infectious patients should be placed in negative pressure rooms. Very often, the HVAC-system with HEPA filters is not capable of reaching this goal. Consequently, other patients, visitors and staff are vulnerable to these infectious agents.
MedicCleanAir® Mobile HEPA Units solve not only the topic regarding infectious agents, but can also equip your hospital with negative pressure rooms. The total working time for such solution is not more than ½ day. – See products, MedicCleanAir® – ISO Concept.
Conclusion:
If you encounter large CFU counts in risk departments with integrated HVAC- systems equipped with or without HEPA filters, contact MedicCleanAir® – we solve the problem.
in our operating theatres
In the past, laminar flow installations were top of the bill to protect the patient that is being operated. Laminar flow installations are supposed to provide clean air in the area of the operating table.
However, multiple medical studies have shown that these installations often only perform in theory and not in practical circumstances. The main reasons are that many devices and hospital staff operate around the operating table and disturb the airflow of the laminar flow installation which in turn brings contaminated air to the patient’s limits.
Additionally, the areas next to the operating table are not purified by this laminar flow system (see drawing – jumper area). Consequently, infections might occur also there, as well as in the preparation or revalidation rooms (the place where the patient is at his weakest point); rooms, which are often not equipped with any HEPA filter system whatsoever.
How to solve the problem:
Install MedicCleanAir® Mobile HEPA Units as these purify the complete operating theatre (not only a certain area is covered, but the complete room)
Conclusion:
Laminar Flow systems in Operating Theatres are often not efficient, or have only a very limited influence on the reduction of airborne infections in O.T.’s.
Note:
Good to know is: that 95% of all operations are successful. The job that the doctor has to do is normally for 95% a success. But when people die, one says ‘he/she did not survive the operation’. The truth is that the patient got infected before or after the operation and died of a complication / infection. Not because the operation went bad.
Usual operating room: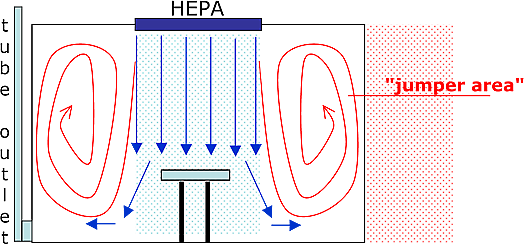
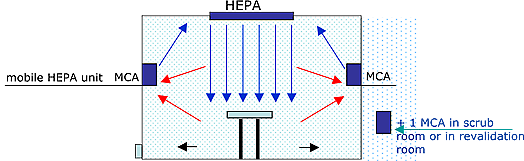
Solution:
MedicCleanAir® PRO units inside the theatre and adjacent areas, MedicCleanAir® ISO 100 or ISO 200 series for the creation of positive pressure.
For detailed information on your specific situation, contact MedicCleanAir®.
Hospital Acquired Infections can be passed on via 3 ways: Contact, food, vector and via air.
Contact is touching something or somebody. A lot of preventive measures have already been implemented to reduce infections by contact; e.g. washing hands 10 times / day, pencils should not accompany the doctor from patient to patient, department to department, door knobs are to be cleaned regularly, etc. etc.
Food is also – or normally is – under control. Nevertheless, sometimes food gets contaminated due to the fact that we all are so much accustomed to the fact that our food chain is clean and completely under control. Often storage and preparation rooms are not clean and disinfected.
Vector is like mosquitos, flies, rats, mouse, cockroaches, etc. which is with good hygiene – normally under control.
Air (including droplets) is more difficult to keep free of contaminants because air is transported from department to department via doors, corridors, HVAC- systems etc.
In the past, keeping air free from contaminants was mostly done by isolating a department from the rest of the hospital, strict hygiene measures, expensive integrated HEPA filtered ventilation systems, expensive laminar flow systems, etc. Nevertheless, these preventive measures of which some are incredible expensive, are always limited to a small area within the hospital and have a very little impact on the reduction of airborne infections.
Air seems to be more and more the ‘transporter’ of hospital infections. It is a fact that very often CFU’s are found in places that have been sterilized before and that have not been touched by anybody. As some of these CFU’s were believed to be passing only by contact, air must be a ‘transporter’ as well.
Proof of this can be found in several medical tests in relation to aspergillosis, and recently the medical studies regarding the fact that MRSA is also airborne.
Solution:
Medical, clinical and laboratory tests have proven that MedicCleanAir® Mobile HEPA Units are the solution to reduce contaminants, infectious agents and the infection rate of patients to zero (see test results).
Air seems to be more and more the main reason for Hospital Infections.
About contact and food, one could do something in the past.
About air one couldn’t – up to now.
For detailed information on your specific situation, contact MedicCleanAir®.
The question of how infections are transmitted has been and often is a major subject of discussions.
The focus is on the transmission through 'contact' as 'contact' is the most obvious way for transmission and consequently the measures are aimed to prevent transmission through 'contact'.
Frequently this results in negligence of the 'airborne' transmission, sometimes even in a denial that there is a link between 'contact' and 'airborne' transmission.
Through the increasing occurrence of MRSA, it has been noted that this attitude is (slightly) changing.
The reason is that, despite severe hygiene and control measures to prevent transmission through contact, MRSA is an increasing problem for hospitals so another option – airborne transmission – has to be considered.
It is likely that also the fact that MRSA has become a subject in the media has contributed to a changing attitude towards 'airborne transmission'.
Since 2002, when the clinical facts on MedicCleanAir® Mobile HEPA Units were published regarding aspergillus concentrations "in the air" – "on surfaces" – "on the floor", following questions are valid:
- What is the reason that material, furniture, medical equipment etc. is contaminated with CFU's when people have not touched it?
- What is the reason that material, furniture, medical equipment etc. is not contaminated with CFU's when MedicCleanAir® has been implemented? 1
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of bacteria that is resistant to certain antibiotics. These antibiotics include methicillin and other common antibiotics such as oxallin, penicillin and amoxillin.
Staph infections, including MRSA, occur most frequently among persons in hospitals and healthcare facilities (such as nursing homes and dialysis centres) who have weakened immune systems. 2
The principle mode of transmission of MRSA is mainly from patient to patient via the transiently colonized hands of healthcare staff.
Healthcare staff acquire the organism:
- through contact with a patient, or
- by handling contaminated surfaces / materials. 3 – 4
Since MRSA has been recovered from many sites, including floors, linen, medical equipment and hospital furniture, consequently transmission via inanimate environments may also be important.
Airborne transmission is generally considered to occur at lower frequency than transmission through direct contact, but MRSA in the form of a bioaerosol can contaminate air and cause airborne infection. 5
Cost of an MRSA infection is estimated between 10.000 and 36.000 Euros. 6
Journal of Hospital Infection (2002) 50; 30 – 35
Evaluation of bed-making related airborne and surface methicillin-resistant Staphylococcus Aureus contamination.
Facts from this publication.
- This study was from August 2000 to July 2001.
- The MRSA patients were in closed, single-patient rooms connected to a central air-conditioning system.
- There were no other activities by personnel and no visitors for an hour before and during bed making.
- Air sampling was done before, during, 15, 30 and 60 min after bed making.
- MRSA containing particles were measured in 6 stages linked to particle sizes
- stage 1 > 7 µm ; stage 2 4.7 – 7.0 µm ; stage 3 3.3 – 4.7 µm
- stage 4 2.1 – 3.3 µm ; stage 5 1.1 – 2.1 µm ; stage 6 0.65 – 1.1 µm
MedicCleanAir®-remark
All sizes meet "airborne infection" qualifications and are transmittable by air to other locations.
The transmission can be to the direct environment for instance the adjacent department but also to other area's of the hospital through the ventilation system.
Sizes from stage 3 – 4 – 5 – 6 / from 0.65 to 4.7 µm are respired, are able to reach the lung.
MedicCleanair® Pro efficiency on MRSA-containing particles is 100 %. 7
MRSA-containing particles were liberated into the air during bed making
MRSA contamination in CFU/m³
- no activity (before bed making) ~ 6
- 30 and 60 minutes after bed making ~ 6
- 15 minutes after bed making ~ 30
- during bed making ~ 116
MedicCleanAir®-remark
Even without any activity, 6 CFU/m³ (MRSA-containing particles) are airborne.
The study – Discussion
"These findings suggest that increase of airborne MRSA during bed making can contaminate the hospital environment and may play a role in MRSA colonization in the nasal cavity, or sequentially, in respiratory MRSA infections. Thus, it is crucial to design an efficient control system to limit the accumulation of MRSA in environments where air is re-circulated. Laminar unidirectional airflow, air ventilation and air filtration could also be beneficial in hospital environments, and should be considered for isolation rooms."
"Although measures for prevention and control of hospital-acquired infection with MRSA include hand disinfection, wearing a gown, gloves, a mask, and removing MRSA from the nasal vestibule, few measures are aimed at control of airborne bacteria".
MedicCleanAir®
From various publications, including Journal of Hospital Infection (2002) 50; 30-35 and its references, it is obvious that MRSA infections require 3 measures to prevent transmission:
- Existing hygiene-measures to prevent transmission through contact should be severely controlled
- MRSA infected patients should be in kept in isolation, and
- The isolation room itself should be equipped with an efficient HEPA air-cleaning system to control MRSA-containing particles: CFU numbers Journal of Hospital Infection (2002) 50; 30 – 35.
Remark
The MedicCleanAir®-ISO Concept offers a workable, economical concept to create A.I.I. (Airborne Infection Isolation) rooms that is very quickly implemented – see concept for Tuberculosis and Sars.
An infectious disease such as Tuberculosis is treated in a specific specialised "Infection" department and here, permanent A.I.I. rooms are required.
MRSA is present in different patient populations, thus in various departments and this makes the discussion on permanent A.I.I. rooms very difficult.
MRSA Facts
MRSA infected patients are to be separated from the environment and kept in isolation.
MRSA-containing particles (CFU) are always present, also when there is no activity. 5
The number of CFU per M³ increase (explode) during activities. 5
MedicCleanAir® recommendation
Installation of 1 MedicCleanAir® PRO in the room where an MRSA-patient is treated.
This will prevent transmission of airborne MRSA contamination, and the patient him/herself will be protected against other (airborne) contamination.
MedicCleanAir® Guidelines
MedicCleanAir® Pro will realise an optimum air quality when following guidelines are met.
- MedicCleanAir® Pro to be installed near the patients' bed on the other bed-side as the door.
- The MedicCleanAir® unit to function at level 1 or 2 during the non-activity period (6 FU/m³).
- The MedicCleanAir® unit to function at level 4 during the bed making procedure and 15 minutes afterwards (the 30 and 116 CFU/m³).
- Door to stay closed during bed making and "some" minutes afterwards.
- "Some" depends on the size of the room (see following note 2).
Note 1
MedicCleanAir® has a 100 % efficiency on all sizes of MRSA-containing particles from 0.65 – 7 µm. 7
Note 2
The efficiency of the MedicCleanAir® filter cartridge and the airflow pattern that is created by the device itself will create and maintain air integrity in the isolation room.
Tests by the University Hospital St. Pierre in Brussels – Belgium – established that MedicCleanAir® required 7 minutes to achieve a 'clean room air-quality' in their isolation-rooms 28 M³.
Note 3
MedicCleanAir® Mobile HEPA Units will not only eliminate the airborne MRSA, but the consequence is that also the risk of contaminated surfaces like medical instruments, furniture etc. will decrease.
What is not in the air cannot sink.
This was proven during a longitudinal study on Invasive Aspergillosis, published by the E.B.M.T.. 6
The sizes of Invasive Aspergillosis equal the sizes of airborne MRSA.
References:
1. Bone Marrow Transplant 29, (2) 2002 – p. 5245 Nº 852
2. Centre of Disease Control (CDC)
3. Infect Control Hosp Epidemiol 1989; 10: 106 – 110
4. Infect Control Hosp Epidemiol 1997; 18: 622 – 627
5. Journal of Hospital Infection (2002) 50; 30 – 35
6. Am. J Infect Control 2002; 30()3): 145 – 152
7. VITO 2000/MIM/R/006
© MedicCleanAir® – 2005
Information:
Journal of Hospital Infection (2002) 50; 30 – 35
Evaluation of bed-making related airborne and surface methicillin-resistant Staphylococcus Aureus contamination.
Sneezing Airborne Spread of MRSA – JID 2006:194 (15 October 2006)
For detailed information on your specific situation, contact MedicCleanAir®.
There exist 4 different types of techniques to ‘filter’ or ‘clean’ the air:
A. The mechanical filtration:
professional technique used in e.g. clean rooms, laminar flow, etc (like MedicCleanAir® does)
B. The electrostatic filtration:
is based on creating electro magnetic fields to attract particles (only particles). Sometimes also equipped with a separate activated carbon filter as final-filter to adsorb gases.
C. Ionisation:
creation of negative ions to maintain an acceptable ratio between positive and negative ions.
D. UV and disinfection:
“killing micro-organisms through UV radiation or through spraying around specific insecticides / chemicals.
See other FAQ’s to see remarks on each filtration technique
This technique adds 'negative' ions (n-ION=energy giving) to the air in order to try to compensate for the 'positive' ions (p-ION=energy eating) that develop through or because of airborne pollution.
The ratio between: (n-ION) and (p-ION)
In the mountains: 3 : 1 (clean fresh air)
In the city: 1 : 500 (polluted air)
n-Ions are available in the air but are eliminated by p-IONS.
p-IONS are created by or develop because of airborne pollution (particles).
What this technique does is not eliminate the p-IONS (negative energy) caused by pollution, but it tries to increase the number of n-IONS which in turn are continuously eliminated by the available p-IONS.
The technique or the ioniser-unit produces n-IONS and does not do anything about the pollution in the air.
A practical example / a comparison:
Take a car that has a hole in its engine and oil is leaking from the engine.
Option 1
To permanently add oil to the engine so that the engine can keep on running.
This could be compared to the ionisation technique.
Option 2
Repair the hole which is taking out p-Ion creator (= factor airborne pollution), which is done by MedicCleanAir®.
Conclusion:
Ionisation techniques are not efficient as they basically do not do anything about airborne pollution (and thus infection control). Medical studies have not shown any positive (short or long term) impact. The technique creates side effects which are even dangerous to immune-compromised patients. (Ozone – see also remarks on electrostatic technique).
Consequently, not to be used in medical facilities.
measure in hospital facilities?
The topic of using UV versus Hepa-filtration as an infection control measure in health care facilities is still very confusing.
CDC guidelines for Environmental Infection Control 2003 and especially page 17 up (= p. 31 of 249) clearly state the following:
“Because the clinical effectiveness of UV systems may vary, UVGI is not recommended for air management prior to air circulation from airborne isolation rooms. It is also not recommended as a substitute for HEPA filtration, local exhaust of air to the outside, or negative pressure. The use of UV lamps and Hepa filtration in a single unit offers only minimal infection-control benefits over those provided by the use of a HEPA filter alone. Duct systems with UVGI are not recommended as a substitute for HEPA filters if the air from isolation rooms must be re-circulated to other areas of the facility. Regular maintenance of UVGI systems is crucial and usually consists of keeping the bulbs free of dust and replacing old bulbs as necessary. Safety issues associated with the use of UVGI systems are described in other guidelines.”
The latest guidelines of CDC 2007 do not mention UV anymore.
In short:
- UV is not recommended anymore by CDC since safety, maintenance, air contact with UV bulbs, etc. is crucial, but more important what CDC states is:
- The clinical effectiveness of UV systems varies a lot between manufacturers.
May each and every manufacturer prove that his particular system (UV or other) is efficient, used in real hospital facilities, under real hospital circumstances, as well as in the short term as in the long run. This can only be proven through medical studies, performed by esteemed professors and hospitals, where the studies are published on a world-wide basis.
As stated by CDC as well, the only reliable sources that one has to support the hospital decisions in relation to infection control guidelines are the multiple medical studies and organisations that prove that a certain device is effective and efficient.
All other statements and brochures of manufacturers are nil, void and give no certainty at all.
Conclusion:
UV is not to be used in medical facilities.
Electrostatic filtration is not used in professional systems (reasons are safety, efficiency and side effects)
'Sold' are 2 main features (advantages vs. mechanical filtration):
- price advantage: manufacturing cost is very low
- no or very low pressure drop: as no filters are installed there is no blockade for the air – a small fan (price!) with a capacity of 100 M³/hour also delivers 100 M³/hour.
Electrostatic filtration and particles
For particles, this technique is a reasonably acceptable under the condition that the device is cleaned about every 48 hours. (High maintenance cost)
If not, there is a decrease in efficiency of about 40%.
Comparison tests in U.S. – mechanical vs. electrostatic –:
After 4 days, the electrostatic technique performed 89% less than the mechanical technique.
Maintenance costs play an important (invisible) role.
Electrostatic filtration and gases
Electrostatic technique does not eliminate gases/chemical compounds.
Note:
Sometimes activated carbon filters are installed in the electrostatic technique as the final filter.
All activated carbon has the tendency to pulverise when becoming saturated.
When pulverising, these small particles are blown into the air creating new pollution.
Electrostatic filtration and its side effects:
The electrostatic technique in itself always creates ozone (which attacks the human immune-system).
When the electrostatic devices are not maintained/cleaned properly, ozone is created in high concentrations.
Electrostatic Units are mostly made out of plastics and therefore contain toxic elements.
Conclusion:
Not suitable for Medical Facilities
1. The casing of a Mobile HEPA Unit:
It is well known that stainless steel (or epoxy anti-bacterial coating) is the only material that is completely safe in relation to maintaining sterile rooms (operating tools, tables, racks, knives, clamps, etc. etc. etc.). Because we are talking Infection Control, it is required that the patients who need Mobile HEPA Units, get the best materials.
If stainless steel was not necessary, it would not be used in hospitals because it is more expensive than plastics and wood.
Plastics are mixed with PCB’s (polychlorische biphenylen) during the fabrication process. These are necessary to get the plastics in the required shape, required form. The look may be nice, but are not to be used hospitals whenever avoidable. These weakening materials are toxic and known to be constantly released by the plastics.
Wooden parts are also treated with all kinds of products before they are installed and used in their final destination (the mobile HEPA unit).
Additionally, both materials are not suitable because germs can stick to the surfaces. As patients need to be surrounded by products and materials that are as less contaminating as possible (must be sterile), only stainless steel is the answer.
Comparison: when we talk about HEPA filtration, we talk about an efficiency of 99.97 % of all particles as small as 0.3 µm or 0.0003 mm. Are we then going to use wood or plastics in devices that need that need to deliver that kind of efficiency ? NO, we are not.
MedicCleanAir® uses stainless steel!
2. The construction of the Mobile HEPA Unit itself:
The contaminated tubes of HVAC-systems are a well known problem in buildings, including hospitals. Constant air humidity and air temperature are the perfect breeding ground for moulds, spores and many other species. It is therefore necessary that the construction of a Mobile HEPA Unit is in such a way that the air inlet and air exhaust is as close to the HEPA Filter as possible. The longer the distance in between, the more risk of growing something within the Mobile HEPA Unit itself.
MedicCleanAir® Mobile HEPA Units are constructed in such a way that the air inlet and air outlet cannot be any closer to the HEPA Filter.
3. The filter itself to be a source of contamination:
MedicCleanAir® Mobile HEPA Units have been medically, clinically and scientifically tested. During these tests, samples were also taken from the clean side of the filter to see if no species have been noted to have grown or passed through the filter. In not one case, these were found on the clean side of the used filter. (change filter cartridge 1x year!)
See also FAQ “Filter questions”
when moved inside the hospital?
Theory:
Efficient Mobile HEPA Units can be used from one department to another without the need of maintenance or change of the filter cartridge.
Advice from MedicCleanAir®:
A Mobile HEPA Unit can perfectly be used in different locations against airborne contamination. However, one should not look for any difficulties or unnecessary risks in the hospital environment. When a Mobile HEPA Unit is used against tuberculosis, keep on using it against tuberculosis, UNLESS MedicCleanAir® (or the agent) has disinfected the Mobile HEPA Unit and has changed the filter cartridge.
This is common sense. Anybody that says that a device can go from tuberculosis to an O.R. or from immune compromised to infectious is not realistic.
Infection Control Units
Although the MedicCleanAir® Mobile HEPA Units have been tested inside, outside, technically, medically and clinically under 'regular' as well as 'severe' (renovation) real hospital conditions, sometimes microbiologists, labs, professors, scientists, etc., want to run extra tests. The reason for this is the need to have additional proof of efficiency of the MedicCleanAir® Mobile HEPA Units in their specific circumstances. This additional proof of efficiency is then included in the file to obtain the necessary funds to acquire the MedicCleanAir® Mobile HEPA Units.
To prevent possible mistakes, incorrect results etc. we cannot stress enough the importance of using the correct procedure to test the MedicCleanAir® Mobile HEPA Units.
The right protocol is required, even for 'quick testing'. The protocol should always be based on the internationally recognised guidelines for testing air purification systems.
There are only 3 ways to do tests in relation to particles:
- taking samples in relation to particles (short term test – few hours/days)
- taking samples in relation to Colony Forming Units – CFU’s (medium term test – few weeks)
- Taking samples that are only part of a complete medical, clinical and microbiological study including all sorts of variables. (long term test – few years)
EN 1822: The standard that greatly impacted the european cleanrooms market. Download the PDF-Article by Thomas Schroth and Dr. Thomas Caesar.
Download >
Airflow is the direction of air
In a negative pressure room, the direction of the air flow is from outside the room to the inside of the room.
In a positive pressure room, the direction of the air flow is from inside the room to the outside of the room.
The more air is extracted or supplied to the room, the stronger the air flow will be.
Pressure difference between a room and the adjacent area
Pressure difference is created when air is being extracted (negative) or supplied (positive) to a very well sealed room. Whenever the room has an opening, grid, integrated A/C, bad sealed windows, bad sealed doors, the creation of pressure difference will be impossible. Even with large amounts of air (extraction or supply), pressure difference will not be accomplished. Only air flow will increase.
Conclusion:
The amount of pressure difference (Pa-difference) depends of the sealing off the room itself. All openings must be sealed before pressure difference can be established.
When pressure difference is not obtained, it does not mean that the isolation room is not working properly. Namely, the air flow is correct and that is the main requirement.
1. Air flow
Air flow is the direction of the air inside the room itself + the direction of the air inside the room in relation to the adjacent areas.
A. Air flow inside the room created by the MedicCleanAir® air purification unit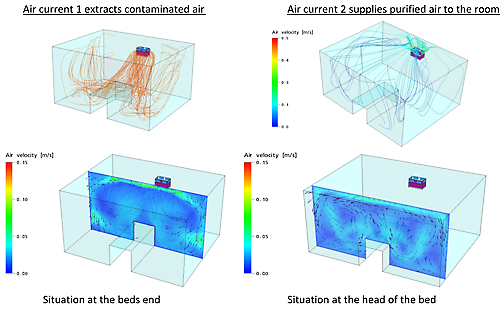
B. Air flow of the air inside the room in relation to the adjacent area.
Picture below: air is extracted at the left corner (bottom floor) + air is being purified by the MedicCleanAir® air purification unit installed against the wall, near the patients bed.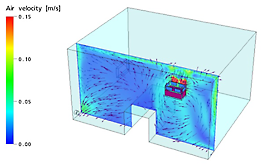
2. Pressure difference between a room and an adjacent area
Pressure difference is the difference between the amount of air inside a room compared to the amount of air inside an adjacent area, expressed in Pascal (Pa). Negative pressure rooms are rooms where there is less air inside the room then outside the room. Positive pressure rooms are rooms where there is more air inside the room then outside the room.
3. Air flow and air purification
In order to purify the air inside a room, the air purification unit must be able to circulate the air inside the room so that the air of every corner of the room is purified and exchanged with purified air. Only then the air quality inside the room is guaranteed. (See drawings A)
4. Air flow and pressure difference
4.1. Negative pressure rooms are rooms with less air inside the room. The air flow in relation to adjacent areas will be from outside the room towards the inside of the room.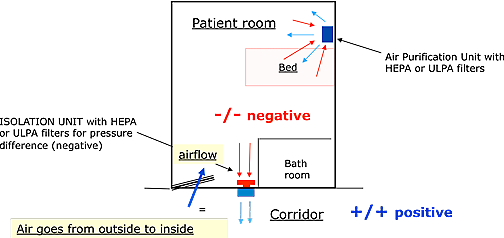
4.2. Positive pressure rooms are rooms with more air inside the room. The air flow in relation to adjacent areas will be from inside the room towards the outside of the room, towards the adjacent areas.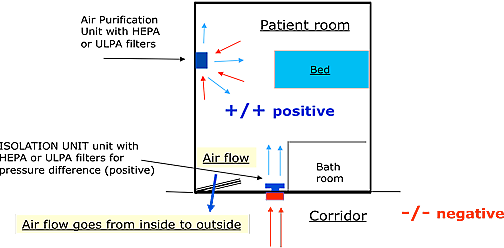
The amount of air that needs to be extracted or supplied to a normal patient room (5x4x2.6 meters) needs to be 100 to 150 m3/hour difference between extraction and supply.
5. Pressure difference itself (negative or positive)
Pressure difference between a room and an adjacent area can only be created when the room itself is sealed off completely. In case there are any leakages, it will be impossible to build up pressure difference. When pressure difference has been achieved, and one creates a leakage (e.g. opening of a door or window), pressure difference will immediately drop to zero and as long as the leakage is there, it will be impossible to build up pressure difference again.
Note: even without pressure difference, air flow can still be correct!
What are leakages that make the creation of pressure difference impossible:
Leakages are openings between the room and adjacent areas where air can float freely. E.g. windows that are not closing well, doors where air can float freely underneath, centralized HVAC-systems that supply cool or heated air, stand alone AC’s with connection to the outside, light fixtures that have openings towards false ceilings, etc.
Comparison:
We blow air into a new balloon. The balloon will have positive pressure inside. Then, we make a hole in the balloon and air will escape through that hole (air flow will be from inside to outside and will continue to be as this as long as air is being pumped inside the balloon – continue to blow the balloon). As a result of the hole, air pressure (the positive pressure inside the balloon) will drop to zero as all air will escape through the hole.
The same counts for rooms where air is being sucked out of (negative pressure rooms). As long as there are no leakages (holes) in that room, pressure difference will be achieved. As soon as leakages occur (holes), pressure difference will not be obtained or if obtained, will fall to zero.
Misunderstanding:
Stating that by increasing the amount of air being pumped inside / or sucked out of a room, one will solve the problem of leakages (holes) inside a room is not correct. As air always goes the easiest way (through holes), enormous ventilation systems with enormous air quantities will be needed to create pressure difference in rooms that are not sealed off well. Additionally in those circumstances, air flow will be very high (≥ 0.2 m/s) and thus influence the comfort (noise and wind draft) of the patient inside the room.
Conclusion:
Isolation rooms (negative or positive) are based on two factors:
- Air quality inside the room
- The direction of the air flow of the air in the room in relation to the adjacent areas, and preferably create pressure difference between the isolation room and the adjacent areas.
One may not simply state that an isolation room is worthless when pressure difference cannot be built up due to leakages. Air quality inside the room can be perfect and the air flow of the air inside the room in relation to the adjacent areas can be correct as well. Thus, isolating patients and protecting hospital staff and visitors in the best way possible. Nevertheless, when rooms are sealed of good, pressure differences of as high as 20 Pascal can be achieved.
MedicCleanAir® – June 2010.
«With the recent outbreak of the deadly Corona virus, it is extremely important for hospitals with isolated infected patients to keep the air in their environment safe and clean. Here is a small appearance of one of our air purification systems reported in the Belgian press this week.»